PhotoCredit_SHVETS production_pexels
Rebound insomnia can strike many who have used prescription sleeping pills. You may find yourself staring at the ceiling after stopping your medication because your brain can’t shift into sleep more without it. Today, we’ll dive into why rebound insomnia occurs and the treatment options including a clinically proven, non-prescription sleep aid that can ease you back into your sleep cycle.
What Is Rebound Insomnia?
Rebound insomnia occurs when an individual experiences new or worsened sleep problems after stopping certain sleep medications. It is closely linked to the discontinuation of drugs like benzodiazepines and other hypnotic agents.
How It Differs from Other Types of Insomnia
Most types of insomnia have underlying causes such as anxiety, chronic stress, medical conditions, or lifestyle factors. Rebound insomnia, however, specifically follows the abrupt cessation or reduction of sleep medications, especially after prolonged use. This can also happen with the sleep aid melatonin.
Unlike primary insomnia, which can persist indefinitely, rebound insomnia tends to be temporary. It often peaks in the first few nights after stopping medication but generally improves with time as the body adjusts. A key feature is that sleep disturbance is more severe than before the medication was started.
This type of insomnia is a direct effect of medication withdrawal rather than an ongoing sleep disorder. It is important to distinguish between long standing issues and a temporary reaction to medication changes.
Rebound Insomnia Prevalence and Risk Factors
The risk of developing rebound insomnia varies based on factors such as the type of medication used, how long it was taken, and individual differences in physiology and psychology.
Benzodiazepines and “Z-drugs” (such as zolpidem) are most commonly associated with rebound insomnia. The risk increases with higher doses and longer durations of use. Sudden discontinuation, rather than gradual tapering, may also increase the likelihood and severity of symptoms.
Certain groups may be at greater risk, including older adults or those with a history of chronic insomnia. Those sensitive to medication withdrawal, or with multiple health conditions, may notice more pronounced effects.
Chart: Key Risk Factors for Rebound Insomnia
| Factor | Influence on Risk |
| Medication Type | Higher with benzodiazepines, Z-drugs |
| Duration of Use | Longer use = higher risk |
| Discontinuation Method | Abrupt stopping increases risk |
| Age | Older adults at higher risk |
| Previous Insomnia | Pre-existing insomnia worsens effects |
Causes of Rebound Insomnia
Rebound insomnia often occurs when individuals stop using certain sleep medications, especially after long-term use. Other risk factors, including the way medications are discontinued and underlying health issues, can also influence the likelihood of experiencing this problem.
Abrupt Discontinuation of Sleep Medications
Abruptly stopping medications used for sleep, particularly those in the benzodiazepine and Z-drug classes, frequently leads to rebound insomnia. These medications alter the brain’s chemistry, so sudden cessation can disrupt natural sleep regulation.
People who have used sleep aids for extended periods or at higher doses face an increased risk. Gradual tapering, under medical supervision, can help reduce the risk and severity of rebound insomnia. For many, withdrawal symptoms go beyond sleep issues and may include anxiety or restlessness.
Most Common Medications for Rebound Insomnia Chart
|
Medication Class |
Examples |
Risk of Rebound Insomnia |
|
Benzodiazepines |
Temazepam, Lorazepam |
High, especially with abrupt stop |
|
Z-Drugs |
Zolpidem, Eszopiclone |
Moderate to high |
|
Antihistamines |
Diphenhydramine |
Low to moderate |
|
Other sedatives |
Trazodone |
Moderate |
Symptoms of Rebound Insomnia
Rebound insomnia often appears after stopping sleep medications and can include:
- Prolonged sleepless nights
- Increased wakefulness above baseline levels
- Intense withdrawal symptoms
- Extreme anxiety
- Body spasms
- Irritability
- Sweating
- Hallucinations
- Depression
- Heart rate changes
Typical Onset and Duration of Rebound Insomnia
Rebound insomnia symptoms usually begin within 1–7 days after discontinuing sleeping medication, particularly with benzodiazepines or non-benzodiazepine hypnotics. However, it can last longer depending on the medication and former dosing. To reestablish your sleep cycle sooner, consider a non-prescription and melatonin-free sleep aid.
The intensity depends on the medication type, dosage, duration of use, and how abruptly the drug was stopped. Gradual tapering off of the medication can reduce severity and shorten duration.
Rebound Insomnia vs Primary Insomnia
While both rebound and primary insomnia share symptoms like difficulty falling asleep or staying asleep, certain differences help distinguish them:Rebound insomnia often manifests as a worsened version of the original sleep issue the drug was prescribed to treat. In contrast, primary insomnia is not linked to medication changes and tends to persist unless addressed with therapy or lifestyle changes.
|
Feature |
Rebound Insomnia |
Primary Insomnia |
|
Cause |
Withdrawal from medications |
Various causes |
|
Onset |
After stopping sleep aids |
May develop gradually |
|
Duration |
Short-term (days to a week) |
Chronic (months or years) |
|
Symptom pattern |
Often more severe initially |
May fluctuate over time |
Daytime Effects
The impact of rebound insomnia is not limited to nighttime. Poor sleep can lead to clear functional impairments during the day.
Common daytime effects include:
- Fatigue and low energy
- Difficulty concentrating or memory problems
- Mood changes such as irritability or anxiety
In severe cases, these symptoms can affect work performance, safety, and quality of life. Even mild rebound insomnia can lead to reduced alertness or a feeling of being mentally “foggy” the next day.
Individuals who develop rebound insomnia may also experience increased worry about sleep, which can contribute to a cycle of ongoing sleep problems if not managed appropriately.
Non Prescription Sleep Aids for Rebound Insomnia
Certain non-prescription sleep aids may provide symptom relief and support more natural sleep patterns for those experiencing rebound insomnia. These options can be particularly relevant for adults seeking alternatives that don’t involve habit-forming medications or prescription drugs.
MDsleep Botanical Sleep Aid
MDsleep Botanical Sleep Aid is formulated with a blend of plant-based ingredients. Key active elements often include valerian root, passionflower, chamomile, and lemon balm. These herbs have a long-standing history of use in supporting relaxation and promoting restful sleep.
It is non-habit-forming and does not contain synthetic sedatives. The supplement aims to help users fall asleep more easily and improve sleep quality without causing significant morning grogginess. People with rebound insomnia may find it beneficial due to its gentle action and low risk of dependence.
MDsleep Botanical Ingredients:
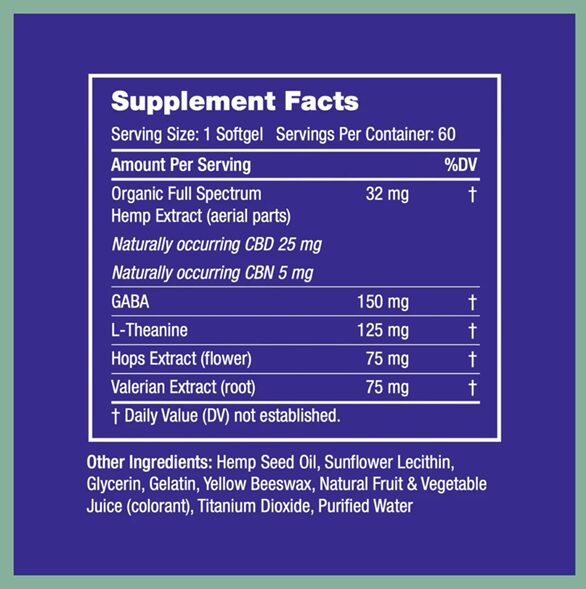
MDsleep + hemp Sleep Aid
MDsleep + hemp Sleep Aid combines traditional botanical ingredients with hemp extract (often in the form of CBD isolate). This formulation is intended for users seeking additional calming benefits from hemp.
The presence of hemp extract may support stress reduction and help reduce nighttime anxiety, which can trigger or worsen rebound insomnia. There is no THC, so users do not experience psychoactive effects or a “high.”
MDsleep + hemp Sleep Aid does not cause dependency and can be used intermittently. Its formulation targets those who want both the benefits of botanicals and the possible calming effects of hemp-derived cannabinoids.
Medications Linked to Rebound Insomnia
Rebound insomnia—worsening sleep trouble after stopping certain drugs—can be triggered by a range of prescription and over-the-counter medications. Different types of sleep aids and sedatives carry varying risk levels and withdrawal effects.
Benzodiazepines
Benzodiazepines are a class of prescription drugs often used to treat insomnia, anxiety, and related conditions. Common examples include diazepam (Valium), alprazolam (Xanax), lorazepam (Ativan), and clonazepam (Klonopin).
These medications act by enhancing the effect of a brain chemical called GABA, leading to sedation and relaxation. When used regularly for more than a few days, the body can quickly become dependent on their sedative effects.
Rebound insomnia tends to occur most often with benzodiazepines that have short half-lives. This means the drug leaves the body quickly, making withdrawal symptoms and sleep disturbances more likely.
Symptoms include difficulty initiating or maintaining sleep, sometimes worse than before starting medication. Tapering off these drugs slowly, under supervision, helps reduce the severity of rebound effects.
Non-benzodiazepine Hypnotics
Non-benzodiazepine hypnotics, also known as “Z-drugs,” include zolpidem (Ambien), zopiclone (Imovane), and eszopiclone (Lunesta). These medications target similar GABA receptors but are structurally different from benzodiazepines.
They are generally prescribed for short-term insomnia relief. Despite their perceived lower dependence risk, withdrawal can trigger rebound insomnia, especially after several days or weeks of use.
Shorter-acting Z-drugs increase the likelihood of rebound effects because their levels drop rapidly. Patients may notice sudden worsening of sleep or even anxiety upon discontinuation. Medical guidance is recommended for tapering or stopping non-benzodiazepine hypnotics.
Over-the-Counter Sleep Aids
Many over-the-counter (OTC) sleep aids contain first-generation antihistamines such as diphenhydramine (Benadryl) or doxylamine. These medications are readily available and commonly used for short-term relief of insomnia.
Prolonged or frequent use of antihistamine-based sleep aids can also lead to tolerance and withdrawal symptoms. In some cases, stopping them suddenly may make it harder to fall or stay asleep, which constitutes rebound insomnia.
OTC sleep aids may also cause side effects like dry mouth, confusion, or daytime drowsiness—especially in older adults. Alternative non-medication strategies for sleep should be considered before relying on these agents.
Rebound Insomnia from Melatonin
Melatonin is a hormone supplement that regulates sleep-wake cycles and is typically considered non-habit-forming. For many people, it poses little risk of withdrawal or rebound effects.
However, individuals using high doses or long-term melatonin supplementation may experience temporary sleep difficulties after stopping. The body’s natural melatonin production can be disrupted, causing mild rebound insomnia until rhythms normalize.
Any sleep disturbance from discontinuing melatonin is usually brief and less severe than withdrawal from prescription sedatives. Still, it is recommended to discuss dosing and duration with a healthcare provider.
Complete list of Rebound Insomnia Associated Medications
The medications most commonly linked to rebound insomnia include:Both prescription and non-prescription medications can be associated with rebound insomnia, particularly when stopped abruptly after regular use. The risk is highest with sedative-hypnotics and drugs that act quickly and leave the body in a short time.
| Drug/Medication Class | Examples |
| Benzodiazepines | Valium, Xanax, Ativan, Klonopin |
| Non-benzodiazepine Hypnotics | Ambien, Lunesta, Sonata |
| OTC Antihistamines | Benadryl, Doxylamine |
| Antidepressants with sedative effects | Trazodone, Mirtazapine |
| Barbiturates | Secobarbital, Pentobarbital |
| Others | Quetiapine (Seroquel), Melatonin |
Shop MDsleep
Find sleep aids that were designed by doctors and validated by research.
Diagnosing Rebound Insomnia
Identifying rebound insomnia requires careful attention to changes in sleep patterns, especially after stopping a sleep medication. Accurate diagnosis depends on recognizing common withdrawal symptoms, tracking sleep behaviors over time, and knowing when to seek professional evaluation.
Recognizing Withdrawal Symptoms
Symptoms of rebound insomnia often appear soon after discontinuing a sleep aid, particularly benzodiazepines or similar drugs. The hallmark sign is a sudden return or worsening of sleep problems that were previously managed by medication.
Key withdrawal symptoms to watch for include:
- Difficulty initiating or maintaining sleep
- Restlessness or anxiety at bedtime
- More frequent or intense awakenings during the night
- A dramatic contrast from pretreatment sleep quality
Not all sleep issues after stopping medication are due to rebound insomnia. Tracking the timing and nature of symptoms can help differentiate between withdrawal effects and other sleep disorders.
Role of Sleep Diaries
Maintaining a sleep diary is one of the most effective ways to monitor and document changes in sleep patterns. Sleep diaries enable individuals to record:A consistent sleep diary helps reveal patterns specific to rebound insomnia, such as abrupt declines in sleep quality directly after stopping medication.
Healthcare professionals may use this information to confirm a diagnosis and distinguish between rebound symptoms and other possible causes.
|
Data to Track |
Examples |
|
Bedtime & Wake Time |
When sleep starts and ends each night |
|
Awakenings |
Frequency, duration, and time of night |
|
Sleep Quality |
Self-rated on a scale (e.g. 1 to 5) |
|
Use of Medications |
Dosages, changes, and timing of last dose |
Short, daily entries are more reliable than relying on memory alone. This objective tracking is key for both personal understanding and clinical assessment.
When to Consult a Healthcare Professional
It is advisable to consult a healthcare professional if sleep disturbances continue for more than a week, worsen, or cause significant daytime impairment. A doctor may ask about recent medication use, sleep habits, and overall health status. They may also review sleep diaries or recommend further assessment, such as a sleep study, to rule out other conditions like sleep apnea.
Prevention Strategies
Reducing the risk of rebound insomnia involves clear steps for stopping sleep medications and exploring alternative techniques to support sleep. Each approach should be based on individual needs and medical guidance for the safest outcomes.
Tapering Off Sleep Medications
Stopping sleep medications abruptly can increase the likelihood of rebound insomnia, especially with benzodiazepines or other sedative-hypnotics. A gradual reduction in dosage, known as tapering, helps the body adjust to lower drug levels.
Healthcare professionals should create a tapering schedule tailored to the specific medication and the person’s medical history. Common tapering strategies include reducing the dose by a set percentage each week or spacing out doses over several days.
Slow tapering allows the brain’s sleep mechanisms to adapt, lessening withdrawal symptoms and minimizing the return of insomnia. During this time, individuals should monitor for signs of anxiety, difficulty sleeping, or withdrawal effects, reporting concerns promptly to their provider.
Alternative Sleep Management Approaches
Non-pharmacological interventions can help support sleep during and after medication tapering. Cognitive behavioral therapy for insomnia (CBT-I) teaches strategies to address thoughts and behaviors that contribute to sleep problems. Relaxation training, sleep hygiene routines, and stress management techniques have shown benefits in clinical studies.
A useful sleep hygiene checklist includes:
- Keeping a consistent sleep schedule
- Limiting caffeine and heavy meals late in the day
- Creating a quiet, dark, and comfortable sleep environment
- Reducing screen time before bed
- Using relaxation techniques such as deep breathing or gentle stretching
Incorporating these methods can reduce dependency on medications and promote long-term improvement in sleep quality.
Treatment of Rebound Insomnia
Rebound insomnia can be managed by targeting both its underlying causes and immediate symptoms. Different approaches range from professional therapies to lifestyle changes and over-the-counter options.
MDsleep + hemp Sleep Aid
MDsleep + hemp Sleep Aid is a non-prescription supplement designed to support sleep, especially during challenging periods such as benzodiazepine withdrawal. This product combines melatonin with a proprietary blend of hemp-derived ingredients. The goal is to help reset natural sleep cycles without causing dependency.
Users may benefit from the following features:
- Non-habit forming formula
- Inclusion of melatonin for circadian rhythm support
- Hemp extract for relaxation benefits
MDsleep + hemp Sleep Aid should be used as directed on the label. Individuals should consult with a healthcare provider before starting new supplements, particularly if taking other medications.
Cognitive Behavioral Therapy for Insomnia (CBT-I)
CBT-I is an evidence-based, drug-free approach proven to help manage insomnia and prevent rebound symptoms. This therapy involves structured sessions, often led by a trained professional, focusing on changing unhelpful thoughts and behaviors related to sleep.
Core components include:
- Sleep restriction: Limiting time in bed to consolidate sleep
- Stimulus control: Creating strong associations between bed and sleep
- Cognitive restructuring: Challenging fears and beliefs about sleep
CBT-I is recommended as a first-line treatment for chronic insomnia. It addresses not only sleep habits but also the psychological factors that contribute to rebound insomnia.
Recovery Timeline for Rebound Insomnia
Rebound insomnia often appears within the first one to two nights after stopping a sleep medication. The intensity and duration can vary depending on the type of medication, its half-life, and individual factors.
|
Duration |
Typical Range |
|
Onset of symptoms |
1–2 nights after stopping |
|
Mild symptoms duration |
2–7 days |
|
Prolonged symptoms |
Up to 4 weeks |
Short-acting medications tend to cause quicker onset of rebound insomnia, but symptoms often resolve more rapidly. For some people, this process lasts only a few days, while others may experience symptoms up to a week.
Longer-acting medications or those taken for a longer period may cause more prolonged rebound insomnia.
Withdrawal symptoms for certain sleep medications, such as benzodiazepines, can sometimes last up to four weeks.
A gradual tapering schedule, supervised by a healthcare provider, can help reduce the severity and duration of rebound insomnia.Not everyone will experience rebound insomnia in the same way. Factors such as dosage, duration of medication use, and a person’s sleep history can influence recovery time.
Frequently Asked Questions
Rebound insomnia often occurs when certain sleep medications are stopped. Sleep disturbances, their duration, and management can depend on the type of medication, withdrawal, and personal factors.
What are the common symptoms of withdrawal-related sleep disturbances?
Symptoms may include difficulty falling asleep, frequent nighttime awakenings, and waking up too early. People can also experience poorer sleep quality than before they started the medication.
Other symptoms might involve vivid dreams, anxiety, and physical restlessness. These issues may be more pronounced in individuals discontinuing certain sedative medications.
How long can one typically expect the sleep disruption to persist after discontinuing sedatives?
Most rebound insomnia symptoms last a few nights up to a week. However, for some, symptoms can persist for several weeks depending on the medication, dosage, and how long it was used.
Gradual dose reduction, or tapering, can help shorten the duration and lessen the severity of sleep difficulties.
Are there effective treatments for managing sleep difficulties post-medication?
Gradually tapering the medication dose is recommended to reduce the risk of rebound insomnia. Cognitive behavioral therapy for insomnia (CBT-I) is also effective for managing ongoing sleep problems after stopping medication.
Sleep hygiene strategies, such as keeping consistent wake times and creating a restful environment, can help improve sleep quality during withdrawal.
Can stopping the use of sleep aids like melatonin trigger difficulty sleeping?
Suddenly stopping melatonin is less likely to cause rebound insomnia compared to prescription sedatives. Some individuals may notice a temporary decline in sleep quality, but significant withdrawal symptoms are uncommon. If problems occur, they are usually mild and short-lived.
What role does alcohol consumption play in the development of sleep issues after cessation?
Alcohol can disrupt sleep patterns, especially when used regularly before bedtime. Stopping alcohol after habitual use can lead to temporary rebound insomnia or increased wakefulness during the night. This effect may be more pronounced in those who used alcohol as a sleep aid.
Is there a difference in how prescription sleep medications and over-the-counter aids affect sleep patterns upon discontinuation?
Prescription sleep medications like benzodiazepines and Z-drugs are more likely to cause rebound insomnia if stopped suddenly. Over-the-counter sleep aids and supplements generally have a lower risk of pronounced withdrawal-related sleep disturbances.
The likelihood and severity of rebound insomnia depend on the specific medication, duration of use, and individual response.
THC for Sleep: Effects and Proper Dose
Learn how THC influences sleep patterns, its potential benefits and risks, and how to determine the right dosage for restful nights. The article provides expert guidance on using THC safely for sleep support.
Read more
CBG vs. CBD: Which Is Right for You?
Uncover the distinctions between CBG and CBD, including their mechanisms of action and potential wellness applications. Learn which cannabinoid may best support your sleep and overall health.
Read more
CBN vs. CBD: Comparing Sleep Benefits
Discover how CBN and CBD differ in their origins, effects, and potential for improving sleep. The article covers their unique properties, legal status, and which might be better suited for your sleep needs.
Read more
CBN for Sleep: How Cannabinol Can Help
Delve into the science behind CBN as a sleep aid, including its sedative properties and how it interacts with your body’s endocannabinoid system. This resource covers dosing, benefits, and considerations for using CBN to improve sleep.
Read more
CBN vs. CBD vs. CBG: A Comprehensive Guide
Compare CBN, CBD, and CBG side by side to see how each cannabinoid affects sleep, pain, and anxiety. Find out which may offer the most benefits for your sleep routine.
Read more
Full Spectrum Hemp: Benefits and Uses
Explore the advantages of full-spectrum hemp, including its diverse cannabinoid profile and potential for promoting better sleep and relaxation. Learn how the “entourage effect” may enhance the efficacy of hemp-based sleep aids.
Read more
CBG vs. CBN: Which Cannabinoid Is Better for Sleep?
Explore the differences between CBG and CBN, two non-psychoactive cannabinoids, and learn how each may impact energy, focus, and sleep quality. This guide discusses their unique effects, benefits, and best uses for rest and relaxation.
Read more

Kia Michel, MD
Physician
Kia Michel, MD is an urologist and staff surgeon at Cedars-Sanai Medical Center in Los Angeles. As a founding member of Comprehensive Urology in Beverly Hills, he believes in treating all aspects of a patient’s wellbeing in order to achieve optimal health. After 25 years in private practice, Dr. Michel believes that a good night’s sleep is essential to maintaining your health, which inspired him to co-create the MDsleep community and the Sleep Doctors Blog.
What Our Readers Say
“Thanks to the insightful articles, I’ve finally managed to get back to my old sleep routine. I feel more rested and energetic each day!”
“The blog’s advice on sleep hygiene has been a game-changer for me. I never realized how small changes could make such a big difference.”
“I struggled with insomnia for years, but the tips I found here have helped me sleep through the night consistently. Thank you!”
“I no longer feel like a zombie from The Walking Dead series! I finally have my life back.”
Stay Updated with Our Newsletter
Join our community of sleep enthusiasts! Subscribe to receive the latest blog posts and exclusive sleep tips straight to your inbox.
Follow Us for More Sleep Insights
Discover Better Sleep Solutions
Unlock the secrets to a restful night by exploring our expert-backed articles and join our vibrant community for personalized sleep tips.
List of References
- OC Revive https://ocrevive.com/rebound-insomnia/
- Summit Behavioral Health https://summithelps.com/withdrawal/sleeping-pills/
- American Journal of Medicine https://www.amjmed.com/article/S0002-9343(13)80001-0/fulltext


